Does Medicare Pay for a Recliner for Seniors? Here’s What Actually Covers It

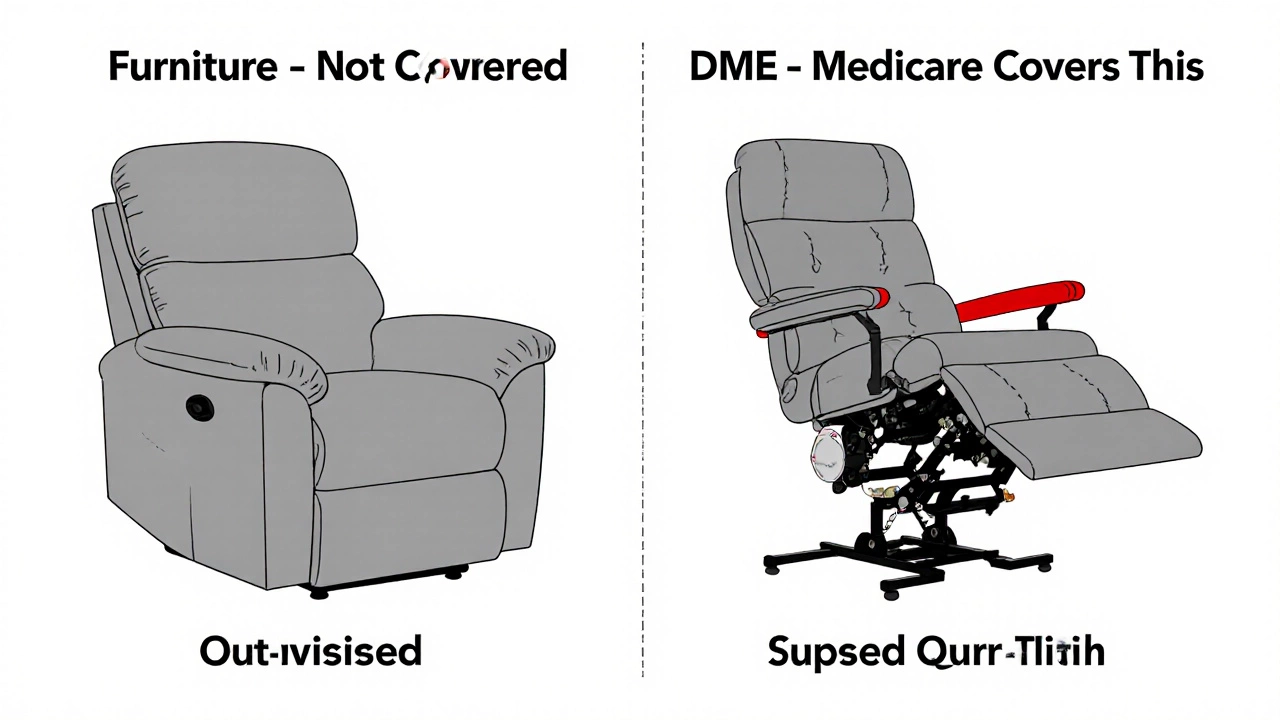
If you’re a senior or caring for one, you’ve probably wondered: Medicare will cover a recliner? The short answer is no - not the kind you find in a showroom. But there’s a twist. If that recliner is medically necessary and meets strict criteria, Medicare might pay for a special type of lift chair - not as furniture, but as durable medical equipment.
Medicare doesn’t cover regular recliners
Medicare won’t pay for a standard recliner, even if it’s expensive or marketed as ‘for seniors.’ That’s because Medicare only covers items classified as Durable Medical Equipment (DME) - tools meant to serve a medical purpose, not improve comfort or convenience. A regular recliner with power tilt and massage features? That’s furniture. Medicare sees it the same way it sees a new sofa: nice to have, but not medically necessary.
Think of it this way: if you bought a recliner because your back hurts and you need to elevate your legs, Medicare won’t cover it unless it’s prescribed as a lift chair with a motorized mechanism that helps you stand up safely. That’s the key difference.
When Medicare might cover a lift chair
Medicare Part B can cover a power lift chair - but only under very specific conditions:
- You have severe arthritis in your hips or knees, or a neuromuscular disease like ALS or MS.
- You’re unable to stand from a regular chair without help.
- Your doctor certifies that the lift chair is medically necessary to improve or maintain your ability to perform daily activities.
- You get the chair from a Medicare-approved DME supplier.
Medicare only pays for the lifting mechanism - not the entire chair. That means they’ll cover the motor, controls, and lift frame, but not the upholstery, cushioning, or style. You’ll pay out of pocket for the rest.
In 2024, Medicare paid an average of $450-$750 for the lift mechanism alone, depending on the model. If the full chair costs $1,200, you’ll pay the difference. And remember: you must have a written prescription from your doctor, and the supplier must accept assignment (meaning they accept Medicare’s approved payment as full payment).
What’s the difference between a recliner and a lift chair?
It’s easy to confuse the two. Here’s how they really differ:
| Feature | Lift Chair | Regular Recliner |
|---|---|---|
| Primary Purpose | Help seniors stand safely | Comfort and relaxation |
| Motorized Lift Function | Yes - raises entire seat | No |
| Medicare Coverage | Possible - for lift mechanism only | No |
| Prescription Required | Yes | No |
| Used in Medical Settings | Yes - often in rehab centers | No |
Some lift chairs come with reclining features too - but that’s just a bonus. The reason Medicare pays for it is the lift, not the recline.
What if you need extra cushioning?
Many seniors need better support for pressure sores, hip pain, or spinal alignment. If you need specialized cushioning, Medicare might cover a therapeutic cushion - but again, only if it’s prescribed as medical equipment.
For example:
- A gel or foam pressure-relieving seat cushion for someone with stage 2 or higher pressure ulcers - covered if prescribed by a doctor.
- A cushion designed to reduce tailbone pain after surgery - may be covered under DME if documented as medically necessary.
These aren’t the same as the $30 memory foam cushions you buy online. Medicare requires documentation showing your condition, the risk of injury without the cushion, and proof that it’s being used for treatment - not comfort.
What about Medicaid or other programs?
Medicare isn’t the only option. If you’re low-income and qualify for Medicaid, your state program may cover more - including full lift chairs or even home modifications like ramps or grab bars. Each state has different rules, so check with your local Medicaid office.
Some nonprofit organizations also help. Groups like the National Association of Area Agencies on Aging (n4a) or local senior centers often have equipment loan programs or grants for seniors who can’t afford necessary devices.
Another option: Veterans Affairs (VA). If you’re a veteran with service-related mobility issues, the VA may cover a lift chair or cushion as part of your benefits.

What to do next
If you think you qualify for coverage, here’s what to do:
- See your doctor. Explain your mobility challenges - how you struggle to stand, how often you fall, or if you’ve had pressure sores.
- Ask for a written prescription for a ‘power lift chair’ or ‘therapeutic seat cushion’ - be specific.
- Call Medicare at 1-800-MEDICARE (1-800-633-4227) to confirm what’s covered and find a DME supplier near you.
- Make sure the supplier is Medicare-approved. You can search the official Medicare supplier directory online.
- Keep all receipts and paperwork. You’ll need them if Medicare asks for proof.
Don’t assume your doctor knows Medicare’s rules. Many don’t. Be ready to explain what you need and why. If your doctor says no, ask for a referral to a physical therapist or occupational therapist - they often have more experience with DME requests.
Common mistakes to avoid
- Buying a lift chair online without a prescription - you’ll pay full price and Medicare won’t reimburse you.
- Choosing a chair based on looks or features like heat or massage - those don’t count for coverage.
- Assuming all ‘senior-friendly’ chairs are covered - most aren’t.
- Not checking if the supplier accepts assignment - if they don’t, you could pay hundreds more.
One real case: A 78-year-old woman in Ohio bought a $1,400 lift chair on Amazon. She didn’t get a prescription. When she submitted the receipt to Medicare, they denied her claim. She had to return it, get the right paperwork, and order through a DME supplier. It took six weeks - but she got the lift mechanism covered.
Alternatives if Medicare won’t cover it
If you don’t qualify for Medicare coverage, there are still ways to get help:
- Try a medical supply rental program - some companies rent lift chairs for $50-$100/month.
- Check with local charities like the Lions Club or Rotary - they sometimes fund mobility aids.
- Use a simple, non-motorized recliner with a sturdy armrest and add a supportive cushion - sometimes that’s enough.
- Look for used DME on Facebook Marketplace or Craigslist - many families sell gently used lift chairs after a loved one passes away or moves to assisted living.
Don’t give up. Mobility matters. Even small changes - like a raised toilet seat or a grab bar near your chair - can make a big difference in safety and independence.
Does Medicare cover lift chairs for seniors?
Yes, but only under strict conditions. Medicare Part B may cover the motorized lift mechanism of a lift chair if it’s prescribed as medically necessary for seniors with severe mobility issues, like advanced arthritis or neuromuscular disease. Medicare does not cover the chair’s upholstery, reclining function, or comfort features - only the lift component.
Can I get a reimbursement for a recliner I already bought?
No. Medicare does not reimburse for equipment bought before getting a prescription and ordering through an approved supplier. You must get the prescription first, then purchase through a Medicare-participating DME provider to be eligible for coverage.
Does Medicare cover memory foam cushions for seniors?
Only if it’s prescribed as a therapeutic cushion for pressure ulcers or other medical conditions. Standard memory foam cushions sold for comfort are not covered. You need a doctor’s note stating the cushion is medically necessary to treat or prevent skin breakdown.
What’s the difference between a lift chair and a recliner?
A lift chair has a motorized mechanism that raises the entire seat to help the user stand up safely. A regular recliner only tilts back and may have a footrest - no lifting function. Medicare only covers the lift mechanism, not the reclining feature.
How much does Medicare pay for a lift chair?
Medicare pays 80% of the approved amount for the lift mechanism, which typically ranges from $450 to $750. You pay the remaining 20% plus any cost above the approved amount for the chair’s frame or upholstery. The total out-of-pocket cost often ends up between $100 and $300 if you choose a basic model.
Do I need a prescription for a lift chair?
Yes. Without a written prescription from your doctor stating the lift chair is medically necessary, Medicare will not cover it. The prescription must include your diagnosis, why the device is needed, and how it improves your ability to perform daily activities.





