Are Seat Cushions Covered by Medicare? Here's What You Really Need to Know

If you're sitting on a hard chair all day and your back or hips ache, you might have thought about getting a seat cushion-especially if you're on Medicare. But does Medicare actually pay for it? The short answer: maybe. It depends on what kind of cushion you need, why you need it, and how it’s prescribed.
Medicare Doesn't Cover Comfort Cushions
Medicare won’t pay for a memory foam cushion you buy off Amazon to make your office chair softer. That’s considered a comfort item, not medical equipment. Medicare only covers items that are deemed durable medical equipment (DME), and only if they’re medically necessary.
Think of it this way: if a cushion is meant to relieve pain from a diagnosed condition like severe arthritis, pressure ulcers, or spinal stenosis, and your doctor says you need it to sit safely, then it might qualify. But if it’s just to make long car rides more pleasant? That’s on you.
What Counts as Durable Medical Equipment?
Medicare defines DME as equipment that:
- Can withstand repeated use
- Has a useful life of at least 3 years
- Is primarily used for a medical purpose
- Is appropriate for home use
- Is not usually useful to someone who isn’t sick or injured
Examples of covered DME include wheelchairs, walkers, oxygen tanks, and hospital beds. Some specialized seat cushions can fall into this category-but only if they meet all five criteria.
When a Seat Cushion Might Be Covered
Medicare Part B may cover a seat cushion if:
- You have a documented medical condition like sacral pressure ulcers (bed sores), severe spinal deformity, or advanced osteoarthritis in the hips or lower back
- Your doctor prescribes it as part of your treatment plan
- The cushion is specifically designed to redistribute pressure and prevent skin breakdown
- You get it from a Medicare-enrolled DME supplier
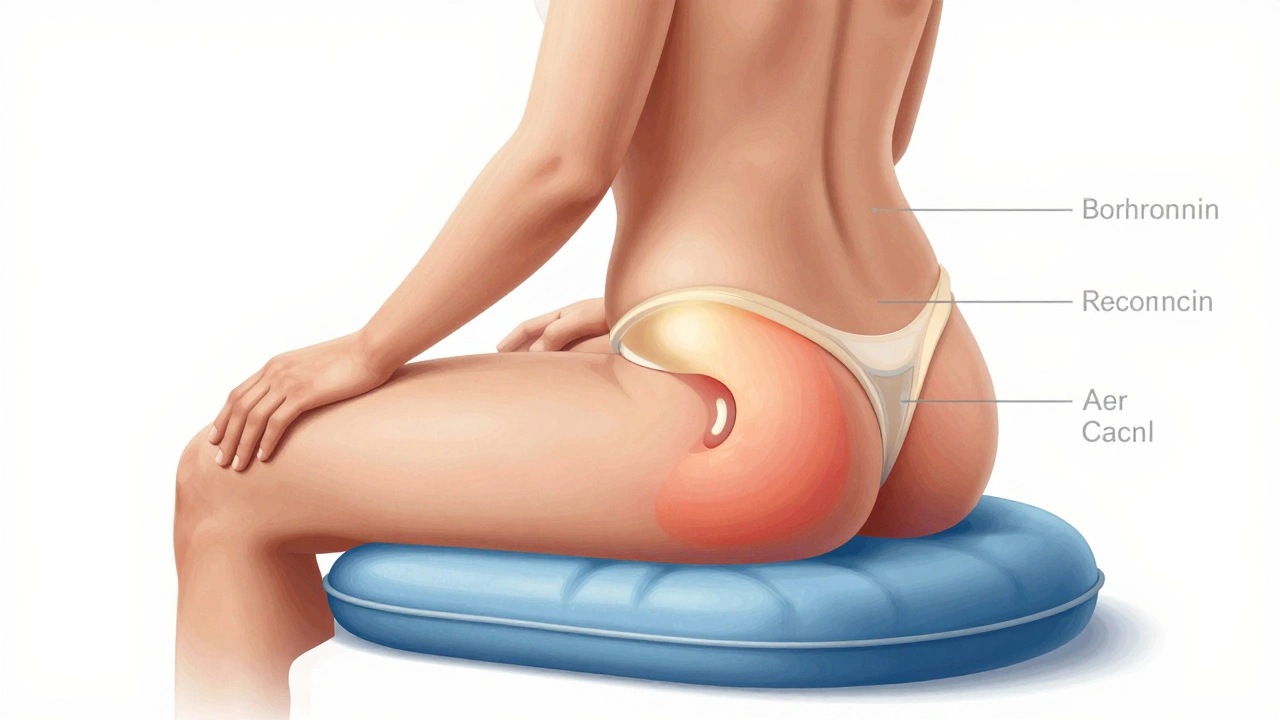
For example, a gel-filled or air-filled pressure-relieving cushion prescribed for someone with spinal cord injury or diabetes-related nerve damage that causes loss of sensation in the buttocks might qualify. These aren’t your average office cushions-they’re medical-grade, often custom-fit, and designed to reduce pressure points that could lead to serious wounds.
What Cushions Are Not Covered
Medicare won’t pay for:
- Memory foam cushions bought online or at a retail store
- Decorative cushions for sofas or chairs
- Cushions marketed for “posture improvement” without a diagnosed condition
- Any cushion without a written prescription from a Medicare-enrolled doctor
- Cushions sold as “ergonomic” without medical documentation
Many websites sell cushions labeled “Medicare-approved,” but that’s misleading. Only the supplier can be Medicare-approved-not the product itself. Always check with your provider before buying.
How to Get Medicare to Cover a Seat Cushion
If you think you qualify, here’s the step-by-step process:
- See your doctor. Explain your pain, mobility issues, or skin breakdown. Bring photos if you have pressure sores.
- Ask your doctor to write a prescription stating the medical necessity. The note must include your diagnosis, why the cushion is needed, and how it will help.
- Find a Medicare-enrolled DME supplier. You can search the Medicare website for suppliers in your area.
- Get the cushion from that supplier. They’ll handle billing Medicare directly.
- Pay your 20% coinsurance. Medicare covers 80% of the approved amount after you meet your Part B deductible.
Don’t buy it yourself and submit a claim later. Medicare rarely reimburses for items purchased outside their network.
What If Medicare Denies Coverage?
Denials happen. Maybe your doctor didn’t include enough detail in the prescription. Or maybe Medicare says your condition doesn’t meet their strict criteria.
If you’re denied, you have the right to appeal. Start by asking for a written explanation of the denial. Then, gather more evidence: physical therapy notes, wound care records, or a second opinion from another doctor. You can file an appeal within 120 days.
Many people get approved on appeal-especially if they show clear medical need with documentation.
Alternatives If Medicare Won’t Cover It
If your cushion doesn’t qualify for Medicare coverage, here are other options:
- Medicaid: Some state Medicaid programs cover DME more broadly than Medicare. Check your state’s rules.
- Veterans Affairs: If you’re a veteran, VA may cover a cushion if it’s related to a service-connected condition.
- Flexible Spending Account (FSA) or Health Savings Account (HSA): You can use pre-tax dollars from these accounts to buy a cushion if your doctor writes a letter stating it’s medically necessary.
- Nonprofits: Organizations like the National Pressure Injury Advisory Panel or local disability groups sometimes offer grants or free equipment.
Some online retailers offer payment plans or discounts for seniors. Look for brands like Roho, Jay, or Varilite-they make medical-grade cushions often used in hospitals and rehab centers.

What to Look for in a Medical-Grade Cushion
If you’re buying one yourself or your insurance covers it, here’s what matters:
- Material: Gel, air, foam, or hybrid systems that adjust to body shape
- Pressure redistribution: Must reduce pressure on bony areas like the tailbone and hips
- Size and fit: Should fit your chair or wheelchair properly
- Cover: Must be washable, non-slip, and breathable
- Medical certification: Look for FDA-cleared or CE-marked products
A cushion that works for someone with spinal cord injury won’t necessarily help someone with hip arthritis. Match the cushion to your specific condition.
Common Misconceptions
Many people believe:
- “All cushions are covered if my doctor says so.” → False. Medicare has strict criteria beyond the prescription.
- “I can buy one and get reimbursed.” → Usually false. Medicare rarely pays for out-of-pocket purchases.
- “If it’s expensive, it’s covered.” → No. Price doesn’t matter-medical necessity does.
- “I can use a cushion from my old wheelchair.” → Maybe, but only if it meets current medical standards and your condition hasn’t changed.
Don’t assume. Always confirm with your provider and supplier.
Bottom Line
Medicare doesn’t cover seat cushions just because you’re uncomfortable. It covers them only if they’re medically necessary to prevent injury or treat a diagnosed condition. If you have pressure sores, nerve damage, or severe joint pain that affects your ability to sit safely, talk to your doctor. Get a proper prescription. Go through a Medicare-approved supplier. And don’t waste money on Amazon cushions labeled “Medicare-approved”-they’re not.
For most people, the right cushion can mean the difference between daily pain and being able to sit through a meal, a doctor’s visit, or a family gathering. It’s not about luxury-it’s about health.
Can I use a seat cushion with my wheelchair and get Medicare to pay for it?
Yes, if the cushion is prescribed for a medical reason like pressure ulcer prevention or spinal support. Medicare covers wheelchair cushions as part of durable medical equipment when they’re medically necessary. You must get it from a Medicare-enrolled supplier and have a doctor’s prescription.
Do I need a prescription for a seat cushion to be covered?
Yes. Without a written prescription from a Medicare-enrolled doctor stating the medical necessity, Medicare will not cover the cushion. The prescription must include your diagnosis, why the cushion is needed, and how it will help your condition.
What if I bought a cushion before getting a prescription?
Medicare generally won’t reimburse you for cushions you bought on your own. To get coverage, you must get the cushion through a Medicare-approved supplier after receiving a valid prescription. Buying ahead of time usually means you pay out of pocket.
Are memory foam cushions covered by Medicare?
Only if they’re medical-grade, prescribed for a specific condition, and purchased from a Medicare-enrolled supplier. Regular memory foam cushions sold for comfort are not covered, even if they’re expensive.
How much does Medicare pay for a covered seat cushion?
Medicare Part B pays 80% of the approved amount after you meet your yearly deductible. You pay the remaining 20%. The exact amount depends on the cushion type and supplier pricing, but most covered cushions range from $150 to $500.
What to Do Next
If you’re struggling to sit comfortably and think a cushion might help, start with your primary care doctor. Don’t wait until you develop pressure sores or your pain gets worse. Get your condition documented. Ask for a referral to a physical therapist or wound care specialist if needed. And always use a Medicare-approved supplier.
It’s not about spending money-it’s about protecting your health. A simple cushion can keep you out of the hospital. That’s worth the effort.





